Bite The Bullet: Oral Blocks Made Easy
Gianluca Bini, DVM MRCVS DACVAA
The use of locoregional techniques allow to block pain in the transmission phase of the nociceptive pathway potentially preventing central sensitization and chronic pain. ¹
When compared to systemic analgesia these techniques provide several benefits including superior intraoperative anesthetic stability and better postoperative pain scores, as well as a lower requirement for postoperative opioids, greater food intake and the potential for cost savings in larger dogs. 2
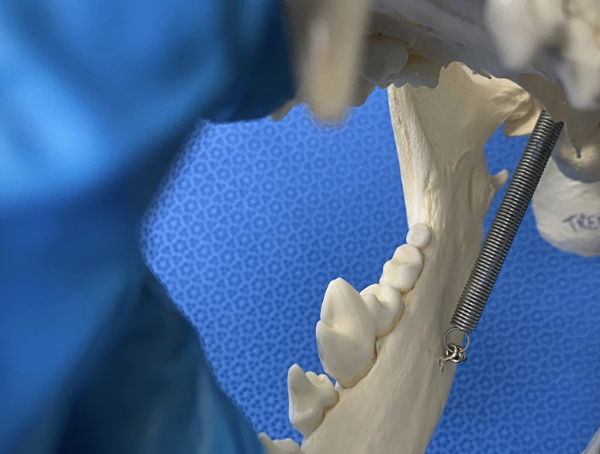
The main innervation of the oral cavity is provided by the maxillary nerve and the mandibular nerve, both of which (together with the ophthalmic nerve) originate from the trigeminal nerve.
Maxillary nerve block
The maxillary nerve innervates the teeth, bone and soft tissue of the maxilla, skin of the nose (including nostrils), upper lip, hard and soft palate as well as the nasal mucosa. The common approaches to the maxillary nerve are either the extraoral, intraoral or infraorbital (not to be confused with an infraorbital block). Most approaches aim at blocking the maxillary nerve as it runs in the pterygopalatine fossa (Fig. 1), which also contains the deep facial vein, the descending palatine artery and the infraorbital artery. Due to the difficulty in identifying the pterygopalatine fossa from outside the patient mouth, it is suggested to perform this nerve block using either the intraoral or infraorbital approaches.
For the intraoral approach the anesthetist will lift the upper lip and then direct the needle perpendicular to the last molar (Fig. 2). Keeping the needle shallow may help decreasing the chances of vascular puncture, in order to successfully block the maxillary nerve the needle only needs to be inserted for few millimeters.
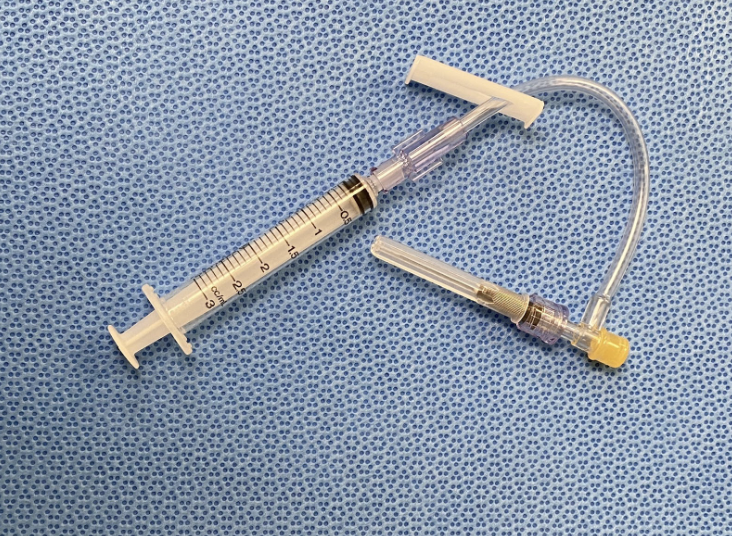
At times this approach may be limited by the logistics of getting the mouth open enough to fit both the needle and the syringe, it is the author preference to use a “T-port” to help (Fig. 3).
Another option is to block the maxillary nerve through the infraorbital canal and injecting a large volume to ensure it would reach the pterygopalatine fossa (Fig 4.).
The infraorbital canal is commonly identified above the third premolars (107/207) and in non-brachycephalic dog breeds it is usually as long as the width of that premolar. In cats the foramen is only few millimeters long, therefore careful advancement of the needle is imperative. In order to identify the infraorbital foramen, it is useful to slide a finger rostro-caudally and feel for a depression, once that’s identified a little neurovascular bundle exiting the canal can be palpated, this contains the infraorbital nerve. For this block an IV catheter can be used (Fig. 5), the anesthetist will slide the catheter in the canal allowing a more precise delivery of local anesthetic and providing an additional layer of safety, preventing the nerve puncture which could be caused if a needle was inserted in the canal.
Infraorbital nerve block
The infraorbital nerve block allows desensitization of the ipsilateral incisors as well as first to third premolars. As previously mentioned, the infraorbital nerve block is performed by identifying the infraorbital foramen above the third premolars (107/207). The anesthetist should slide a finger rostro-caudally while feeling for a depression, once that’s identified a little neurovascular bundle exiting the canal can be palpated, this contains the infraorbital nerve. While in non-brachycephalic dog breeds it is usually as long as the width of that premolar, in cats the foramen is only few millimeters long, therefore careful advancement of the needle is imperative in this specie. For this block a needle (Fig. 6) can be used without much risk as local anesthetic is just deposited at the level of the foramen.
Mandibular nerve block
The mandibular nerve innervates the mandibular teeth, bone and soft tissue including the lower lip. This nerve block is performed with an extraoral approach, it is only advised for radical procedures (e.g. mandibulectomies) and the anesthetist will need a nerve stimulator to confirm the correct placement of the needle. The needle is advanced rostromedially at the level of the temporomandibular joint while looking for the muscle response elicited by the nerve stimulator, making this block more complicated to perform in most settings. 3 This block should be performed only on one side, due to the risk of tongue self-mutilation.
Inferior alveolar nerve block
The inferior alveolar block will desensitize the ipsilateral mandible body cranial to the foramen, the lower dental arch and the lower lip. In the author opinion it is easier to perform this block intraorally. To identify the inferior alveolar nerve, the anesthetist can use a finger to identify the mandibular arch, then slide the finger dorso-ventrally, at that point the mandibular foramen and a small neurovascular bundle can be palpated, this contains the inferior alveolar nerve. The local anesthetic can be injected rostrally to the bundle paying attention to not puncture it. In cats the foramen is harder to identify as it has a smaller and shallower opening. This is another nerve block where the author prefers to use a “T-port” to help with logistics (Fig. 3).
As per the mandibular nerve block, it is advised to perform this block only on one side, due to the risk of tongue self-mutilation.
Tongue self-mutilation
Usually occurs when the patient is dysphoric, it is advised to sedate the patient while holding the patient mouth closed, if possible, to prevent further damage. Once sedated closely examine the tongue and treat appropriately. A slow recovery in a quiet environment may help prevent this.
Mental nerve block
The inferior alveolar block will desensitize the ipsilateral mandible body cranial to the foramen, as well as the dental arch cranial to the foramen. The mental foramen can be located ventral to the 2nd premolar (Fig. 9), at that location the anesthetist will slide a finger rostro-caudally, and a neurovascular bundle exiting the foramen can be palpated. Local anesthetic can be injected rostrally to the foramen.
Needle selection
A 22 or 20-gauge hypodermic needle can be used to perform most oral blocks injections. It is advised to use a T-port to facilitate the positioning of the needle (Fig. 3). A 22 or 24-gauge IV catheter can be used for the infraorbital nerve block.
Drug and volume selection
Drug choice for oral blocks depends on the required length of analgesia.
A local anesthetic can be used together with epinephrine or an alpha-2 agonist to prolong and enhance depth of the blockade. A few examples of drug choices are presented in Table 1. The maximum suggested doses are reported.
| Drug name | Maximum dose | Onset (min) | Duration (h) |
|---|---|---|---|
| Lidocaine | 4mg/kg | 2-3 | 1-2 |
| Bupivacaine | 2mg/kg | 6-10 | 3-6 |
| Ropivacaine | 3mg/kg | 6-10 | 2-4 |
| Bupivacaine + Dexmedetomidine |
1mg/kg + 0.001mg/mL | 10 | Up to 24h |
| Bupivacaine + Epinephrine | 2mg/kg + 0.005mg/mL | 10 | Up to 12h |
Typically, 0.5 mL of 0.5% ropivacaine/bupivacaine can be used for most oral blocks in a dog below 10Kg of body weight while 1mL of 0.5% ropivacaine/bupivacaine can be used in dogs above 10Kg of body weight. On the other hand, 0.5 mL of 0.5% ropivacaine/bupivacaine is sufficient for oral blocks in cats.
Ideally, the maximum total injected volume should be calculated first, then the dose of the adjunct (if used) and ultimately the dose of local anesthetic. If the volume of the adjunct plus local anesthetic exceeds the total injected volume desired, the amount of local anesthetic can be decreased to fit within the volume limit.
It is always advised to withdraw before injecting when attempting any injection, most nerves have significant vascular structures in the surrounding area and intravascular injection of local anesthetics should be avoided at all costs. Inadvertent intravascular injection could lead to a spike in local anesthetic plasma concentration and hence local anesthetic toxicity.
Role of inflammation and mixtures of local anesthetics
Local anesthetics are weak bases, when injected part of them are in a ionized and unionized form. Only the unionized form can enter the axon and block the sodium channels from inside the nerve. The amount of local anesthetic in each form is determined by the local anesthetic pKa and the local tissue pH. 6 The pKa is the local tissue pH at which the ionized and unionized forms exist in equal concentrations. Local anesthetics with a pKa closer to a physiologic pH will have more molecules in the unionized form and vice versa. 6 If a tissue is inflamed its pH will be lower hence there will be less local anesthetic molecules in the unionized form, making the local block less effective (or completely ineffective). 6
Moreover, it is not advised to mix different local anesthetics this will alter their properties with no practical benefit, for example studies demonstrate a mixture of lidocaine (pKa 7.8 ) and bupivacaine (pKa 8.1) did not have a faster onset but had a shorter duration than bupivacaine alone. 7
References
Latremoliere, A., & Woolf, C. J. (2009). Central sensitization: a generator of pain hypersensitivity by central neural plasticity. The Journal of Pain, 10(9), 895–926.
Palomba, N., Vettorato, E., Gennaro, C. De, & Corletto, F. (2020). Peripheral nerve block versus systemic analgesia in dogs undergoing tibial plateau levelling osteotomy: Analgesic efficacy and pharmacoeconomics comparison. Veterinary Anaesthesia and Analgesia, 47(1), 119–128.
Otero, P.E. and Portela, D.A., 2019. Small animal regional anesthesia, 2nd ed.
Otero, P.E. and Campoy, L., 2013. Small animal regional anesthesia and analgesia.
Bartel, A.K., Campoy, L., Martin-Flores, M., Gleed, R.D., Walker, K.J., Scanapico, C.E. and Reichard, A.B., 2016. Comparison of bupivacaine and dexmedetomidine femoral and sciatic nerve blocks with bupivacaine and buprenorphine epidural injection for stifle arthroplasty in dogs. Veterinary Anaesthesia and Analgesia, 43(4), pp.435-443.
Lawal FM, Adetunji A. A comparison of epidural anaesthesia with lignocaine, bupivacaine and a lignocaine-bupivacaine mixture in cats. J S Afr Vet Assoc. 2009;80(4):243-246.
Lizarraga I, Janovyak E, Beths T. Comparing lidocaine, bupivacaine and a lidocaine-bupivacaine mixture as a metacarpal block in sheep. Vet J. 2013;197(2):515-518.
Continue Reading